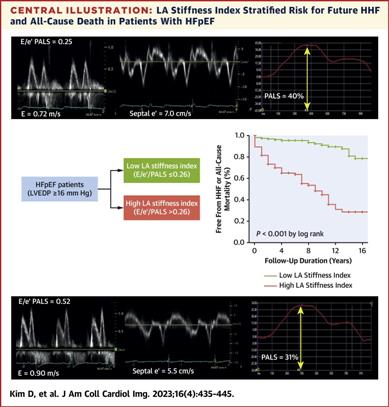
Prognostic Implications of Left Atrial Stiffness Index in Heart Failure Patients With Preserved Ejection Fraction |
| |
| Affiliation: | 1. Division of Cardiology, Department of Internal Medicine, Heart Vascular Stroke Institute, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea;2. Division of Cardiology, Department of Internal Medicine, Kangwon National University Hospital, Kangwon National University School of Medicine, Chuncheon, Republic of Korea;3. Division of Cardiology, Department of Internal Medicine, Chonnam National University Hospital, Gwangju, Republic of Korea;4. Department of Critical Care Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea |
| |
| Abstract: | 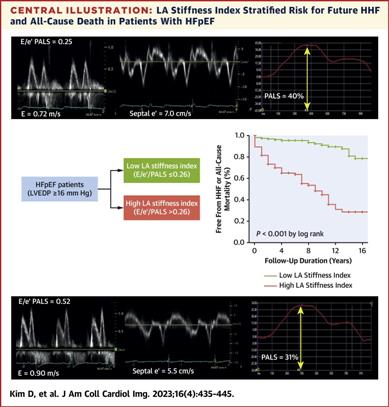
BackgroundThe left atrium (LA) plays an important role in the pathophysiology and disease progression of heart failure with preserved ejection fraction (HFpEF).ObjectivesThis study sought to assess the prognostic potential of LA stiffness index in patients who have HFpEF.MethodsThis study retrospectively screened patients with elevated left ventricular end-diastolic pressure (≥16 mm Hg) and preserved ejection fraction (≥50%) between January 1, 2004, and December 31, 2019. All patients underwent left heart catheterization to measure left ventricular end-diastolic pressure. Among these, 307 patients who had suitable image quality for left peak atrial longitudinal strain (PALS) measurement were analyzed. The study population was classified into low LA stiffness (n = 178, early diastolic transmitral inflow velocity/mitral annulus early diastolic velocity [E/e′]/PALS ≤0.26) and high LA stiffness (n = 129, E/e′/PALS >0.26) according to the best LA stiffness index (E/e′/PALS) cutoff value. The primary outcome was a composite of mortality or hospitalization caused by heart failure during follow-up.ResultsLA stiffness index showed good correlations with E/e′ (r = 0.737; P < 0.001), LA volume index (r = 0.529; P < 0.001), right ventricular systolic pressure (r = 0.404; P < 0.001), and log N-terminal pro–B-type natriuretic peptide (r = 0.540; P < 0.001). LA stiffness index demonstrated better predictive performance than echocardiographic diastolic parameters did (P < 0.001). Patients with low LA stiffness had better clinical outcomes than those with high LA stiffness during a median follow-up of 6 years did (P < 0.001). In multivariable analysis, LA stiffness index was independently associated with increased risk of the composite endpoint of death or heart failure hospitalization (HR: 1.59 [95% CI: 1.01-2.51]; P = 0.044).ConclusionsIncreased LA stiffness was associated with increased risk for all-cause mortality and hospitalization caused by heart failure in patients who have HFpEF, and its prognostic role was more pronounced than that of indexes of left ventricular filling pressure. |
| |
| Keywords: | left atrial stiffness left atrial strain left ventricular filling pressure prognosis AUC" },{" #name" :" keyword" ," $" :{" id" :" kwrd0035" }," $$" :[{" #name" :" text" ," _" :" area under the curve E/e′" },{" #name" :" keyword" ," $" :{" id" :" kwrd0045" }," $$" :[{" #name" :" text" ," _" :" early diastolic transmitral inflow velocity/mitral annulus early diastolic velocity HFpEF" },{" #name" :" keyword" ," $" :{" id" :" kwrd0055" }," $$" :[{" #name" :" text" ," _" :" heart failure with preserved ejection fraction LA" },{" #name" :" keyword" ," $" :{" id" :" kwrd0065" }," $$" :[{" #name" :" text" ," _" :" left atrium LV" },{" #name" :" keyword" ," $" :{" id" :" kwrd0075" }," $$" :[{" #name" :" text" ," _" :" left ventricle LVEDP" },{" #name" :" keyword" ," $" :{" id" :" kwrd0085" }," $$" :[{" #name" :" text" ," _" :" left ventricular end-diastolic pressure NT-proBNP" },{" #name" :" keyword" ," $" :{" id" :" kwrd0095" }," $$" :[{" #name" :" text" ," _" :" N-terminal pro–B-type natriuretic peptide PALS" },{" #name" :" keyword" ," $" :{" id" :" kwrd0105" }," $$" :[{" #name" :" text" ," _" :" peak atrial longitudinal strain ROC" },{" #name" :" keyword" ," $" :{" id" :" kwrd0115" }," $$" :[{" #name" :" text" ," _" :" receiver-operating curve TR" },{" #name" :" keyword" ," $" :{" id" :" kwrd0125" }," $$" :[{" #name" :" text" ," _" :" tricuspid regurgitation |
| 本文献已被 ScienceDirect 等数据库收录! |
|