Trends in axillary surgery and clinical outcomes among breast cancer patients with sentinel node metastasis |
| |
| Affiliation: | 1. Department of Breast Surgery, West China Hospital, Sichuan University, Chengdu, People''s Republic of China;2. State Key Laboratory of Biotherapy and Cancer Center, West China Hospital, Sichuan University, Chengdu, People''s Republic of China;3. Department of Pathology, West China Hospital, Sichuan University, Chengdu, People''s Republic of China;4. Institute of Clinical Pathology, West China Hospital, Sichuan University, Chengdu, People''s Republic of China;5. West China School of Medicine/West China Hospital, Sichuan University, Chengdu, People''s Republic of China |
| |
| Abstract: | 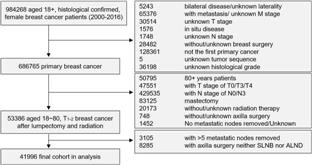
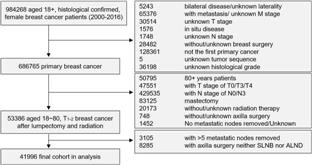
BackgroundThere is a lack of studies examining the long-term trend and survival of axillary surgery for breast cancer patients with sentinel node metastasis, especially for the patients with 3–5 node metastases.MethodsBreast cancer patients with 1–5 sentinel node metastases from the Surveillance, Epidemiology, and End Results (SEER) database from 2000 to 2016. Our study presented the trend of axillary surgery and assessed the long-term survival of sentinel lymph node biopsy (SLNB) alone vs axillary lymph node dissection (ALND) for those patients.ResultsOf the 41,996 patients diagnosed with T1-2 breast cancer after lumpectomy and radiation included, 34,940 had 1-2 sentinel node metastases and 7056 had 3-5 sentinel node metastases. The percentage of patients undergoing SLNB alone increased from 22.4% in 2000 to 81.0% in 2016 for patients with 1–2 sentinel node metastases, and quadrupled from 5.2% in 2009 to 20.6% in 2016 for those with 3–5 sentinel node metastases. Completion of ALND did not benefit the long-term survival of 1–2 sentinel node metastasis patients (hazard ratio [HR] = 1.02, P = 0.539), but improved the long-term survival of 3–5 node metastasis patients (HR = 0.73, P < 0.001). Subgroup analysis demonstrated the inferiority of SLNB to ALND in all subgroups of 3–5 sentinel node metastases.ConclusionFor patients with T1-2 breast cancer after lumpectomy and radiation, SLNB alone was an efficient and safe surgical choice for 1–2 sentinel node metastases but not for 3–5 sentinel node metastases. It is worth noting that for patients with 3–5 node metastasis, the proportion of omitted ALND quadrupled after 2009. |
| |
| Keywords: | Sentinel lymph node biopsy Axillary lymph node dissection Sentinel node metastasis Overall survival |
| 本文献已被 ScienceDirect 等数据库收录! |
|