The evaluation of sleep disturbances for Chinese frontline medical workers under the outbreak of COVID-19 |
| |
| Affiliation: | 1. School of Medicine, Nankai University, Tianjin, 300071, China;2. Department of Neurology, The Secondary Medical Center, Sleep Medicine Research Center, Chinese PLA General Hospital, Beijing, 100853, China;3. Department of Neurology, Union Hospital, Tongji Medical College, Huazhong University of Science & Technology, Wuhan, Hubei, 430022, China;4. Department of Neurology, Tongji Hospital, Tongji Medical College, Huazhong University of Science & Technology, Wuhan, Hubei, 430030, China;5. Department of Neurology, Renmin Hospital of Wuhan University, Wuhan, Hubei, 430060, China;6. Department of Neurology, Zhongnan Hospital of Wuhan University, Wuhan, Hubei, 430071, China;7. Department of Neurology, The Central Hospital of Enshi Tujia and Miao Autonomous Prefecture, Enshi, Hubei, 445000, China;8. Department of Neurology, Jingzhou Central Hospital, Jingzhou, Hubei, 434000, China;9. Department of Neurology, Huanggang Central Hospital, Huanggang, Hubei, 438000, China;10. Department of Neurology, People''s Hospital of Yichang Central, Yichang, Hubei, 443003, China;11. Department of Neurology, Xiangyang Central Hospital, Xiangyang, Hubei, 441021, China;12. Department of Neurology, Red Cross Hospital of Wuhan, Wuhan, Hubei, 430015, China |
| |
| Abstract: | 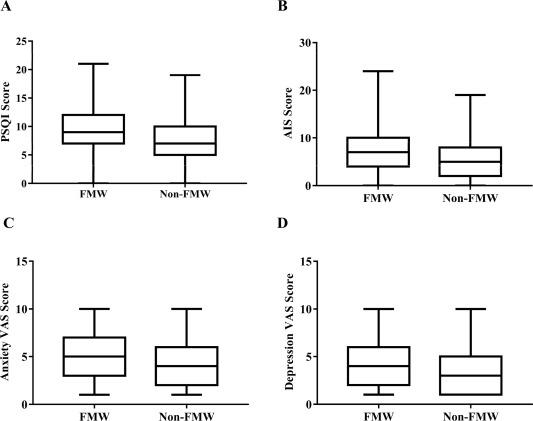
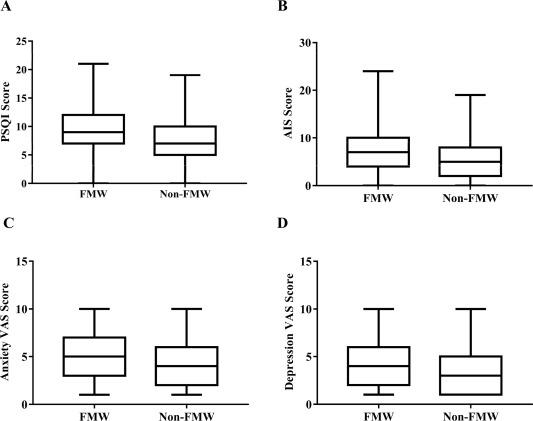
ObjectiveTo evaluate sleep disturbances of Chinese frontline medical workers (FMW) under the outbreak of coronavirus disease 2019 (COVID-19), and make a comparison with non-FMW.MethodsThe medical workers from multiple hospitals in Hubei Province, China, volunteered to participate in this cross-sectional study. An online questionnaire, including Pittsburgh Sleep Quality Index (PSQI), Athens Insomnia Scale (AIS) and Visual Analogue Scale (VAS), was used to evaluate sleep disturbances and mental status. Sleep disturbances were defined as PSQI>6 points or/and AIS>6 points. We compared the scores of PSQI, AIS, anxiety and depression VAS, as well as prevalence of sleep disturbances between FMW and non-FMW.ResultsA total of 1306 subjects (801 FMW and 505 non-FMW) were enrolled. Compared to non-FMW, FMW had significantly higher scores of PSQI (9.3 ± 3.8 vs 7.5 ± 3.7; P < 0.001; Cohen's d = 0.47), AIS (6.9 ± 4.3 vs 5.3 ± 3.8; P < 0.001; Cohen's d = 0.38), anxiety (4.9 ± 2.7 vs 4.3 ± 2.6; P < 0.001; Cohen's d = 0.22) and depression (4.1 ± 2.5 vs 3.6 ± 2.4; P = 0.001; Cohen's d = 0.21), as well as higher prevalence of sleep disturbances according to PSQI > 6 points (78.4% vs 61.0%; relative risk [RR] = 1.29; P < 0.001) and AIS > 6 points (51.7% vs 35.6%; RR = 1.45; P < 0.001).ConclusionFMW have higher prevalence of sleep disturbances and worse sleep quality than non-FMW. Further interventions should be administrated for FMW, aiming to maintain their healthy condition and guarantee their professional performance in the battle against COVID-19. |
| |
| Keywords: | Sleep disturbances COVID-19 Pressure Medical workers COVID-19" },{" #name" :" keyword" ," $" :{" id" :" kwrd0035" }," $$" :[{" #name" :" text" ," _" :" Coronavirus disease 2019 FMW" },{" #name" :" keyword" ," $" :{" id" :" kwrd0045" }," $$" :[{" #name" :" text" ," _" :" Frontline medical workers PSQI" },{" #name" :" keyword" ," $" :{" id" :" kwrd0055" }," $$" :[{" #name" :" text" ," _" :" Pittsburgh Sleep Quality Index AIS" },{" #name" :" keyword" ," $" :{" id" :" kwrd0065" }," $$" :[{" #name" :" text" ," _" :" Athens Insomnia Scale VAS" },{" #name" :" keyword" ," $" :{" id" :" kwrd0075" }," $$" :[{" #name" :" text" ," _" :" Visual Analogue Scale |
| 本文献已被 ScienceDirect 等数据库收录! |
|